Cultural competence:
“The ability to understand, communicate with and effectively interact with people across cultures.”
(Livingstone, 2016).
According to the article What does it mean to be culturally competent? (n.d). there are three levels of cultural competence, which consist of 1) awareness, 2) knowledge, 3) skills. These are always changing in response to new situations, personal growth, relationships and experiences.
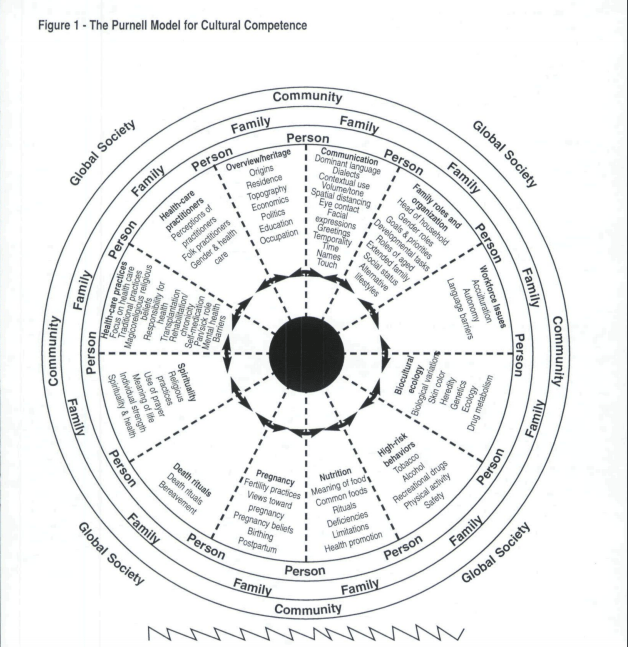
Cultural competence in healthcare can also be defined using the Purnell model. The purpose of this model is to:
- Provide a framework for all healthcare providers to learn concepts and characteristics of culture
- Define circumstances that affect a person’s cultural worldview in the context of historical perspectives
- Provide a model that links the most central relationships of culture
- Interrelate characteristics of culture to promote congruence and to facilitate the delivery of consciously sensitive and competent health care
- Provide a framework that reflects human characteristics such as motivation, intentionality, and meaning
- Provide a structure for analyzing cultural data
- View the individual, family, or group within their unique ethnocultural environment.
The Purnell model can be found here!
What does it mean to be culturally competent?
Cultural competence has several characteristics and includes knowledge and skills as well as the following:
• Developing an awareness of one’s own culture, existence, sensations, thoughts, and environment without letting them have an undue influence on those from other backgrounds
• Demonstrating knowledge and understanding of the client’s culture, health-related needs, and meanings of health and illness
• Accepting and respecting cultural differences
• Not assuming that the healthcare provider’s beliefs and values are the same as the client’s
• Resisting judgmental attitudes such as “different is not as good;” and
• Being open to cultural encounters and being comfortable with cultural encounters
• Adapting care to be congruent with the client’s culture
• Cultural competence is an individualized plan of care that begins with performing an assessment through a cultural lens
Cultural considerations at end-of-life
Reflection
Understanding cultural competence has changed my view of healthcare, as before this course, working at a rural hospital I felt that I was not subjected to enough culture. Now, I understand that culture is not just visibly seen. It is someones beliefs, habits, behaviours, rituals etc. Being culturally competent is about understanding different cultures, respecting their wishes and being aware of your own self in the process. I participated in discussion postings for the course and created a peerwise question based on communication, which involved creating a plan of care for the patient that would be culturally specific and accommodating. I also found that attending live sessions each week allowed me to ask questions first hand and receive feedback right away from my teacher.
My peerwise question during the course:
You are working on a complex continuing care unit and receive a new admission. Your patient is an 82 year old female who only speaks Romanian. This patient does not understand English and you don’t have any health care providers at the hospital that speak her language. To effectively complete your admission assessment and care for the patient, which of the following is effective?
A – Use non-verbal communication to complete the admission
B – Ask questions in English and write down what you think the patient is saying
C – Call for an interpreter to come in and translate
D – Leave the patient alone until family comes
My Explanation:
While using non-verbal communication can be an effective way for communication when there are language barriers, it is not acceptable when first meeting a patient and completing an admission assessment on them. In order to provide care for this patient, there needs to be communication between the nurse and the patient that is correct, and that consent can be given by the patient for the care at the hospital.
The CNO states “Interpreters are essential when a nurse-patient language barrier exists. When using interpreters to communicate with patients, you need to obtain patient consent, be sensitive to the issues surrounding interpretation and ascertain the interpreter’s appropriateness for the particular patient situation. You also are encouraged to consult with your employer regarding organizational policies on using interpreters and work with your employer to develop policies if none are in place.” (2018).
References:
The College of Nurses of Ontario (2018). Culturally sensitive care. Retrieved from:https://www.cno.org/en/learn-about-standards-guidelines/educational-tools/ask-practice/culturally-sensitive-care/
Purnell, L. (2005). The Purnell Model for Cultural Competence. Retrieved from https://files.midwestclinicians.org/sharedchcpolicies/Policies_Forms/Cultural Competency/PURNELL’S MODEL.pdf.
Livingstone, R. (2016). What does it mean to be culturally competent? Retrieved from https://wehearyou.acecqa.gov.au/2014/07/10/what-does-it-mean-to-be-culturally-competent/.
Rexdale Womens Centre (n.d). What does it mean to be culturally competent? Retrieved from http://rapworkers.com/wp-content/uploads/2017/08/what-does-it-mean-to-be-culturally-competent-1.pdf
